

Building Worlds Beyond Ours: bib sama. and Tayoloxs in Conversation on GAIA, Escapism, and the Future of the Underground
At a time when the weight of the world feels heavier than ever, the art of world-building has become an act of resistance — and few are doing it quite like bib sama. and Tayoloxs. Over the past year, the two emerging London visionaries have been constructing a sonic universe around their forthcoming project, GAIA — not just through sound, but through community. Working with a constellation of collaborators — from the emerging cinematographer Rino, to the visual artist SIMMS,


Aitch Speaks on Being a Northern Soul With a Southern Spirit Blending Comfort & Style
Southern comfort has teamed up with Manchester’s Local Space for a limited-edition streetwear drop, Northern Comfort, a line fronted by the renowned Brit Award Winning artist, Aitch.

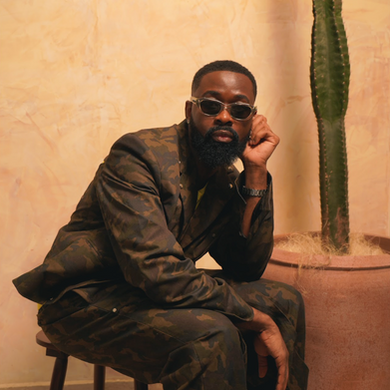
Definition of Protect Sarz At All Costs, His Debut Album, and Upcoming Collaboration With Rema [Interview]
Bringing in artistes from various continents, the 12-track body of work was released on the 25th of September.


The Hitmaker Series: KTmelodies On The Winding Road To Stardom
KTmelodies is a multi-instrumentalist, producer, and rapper influenced by electronic artists like David Guetta, Disclosure, and Kaytranada. Having crafted some impressive early releases that blend genres, his single "Pack Up Ya Bags" gained significant attention.


Khamari Unravels The Complexities of Humanity on His Sophomore Album, To Dry A Tear
Having quietly evolved into one of the most compelling new voices in contemporary R&B, Boston-born,Los Angeles-based artist Khamari has released his second full length album, To Dry A Tear.















Comments